Blocking immune checkpoints as well as modifying T-cells could be a promising treatment approach for melanoma, according to two new studies conducted by researchers at the Clinical Research Division of the Fred Hutch Cancer Research Center in Seattle, Washington.
The studies, “T-Cell Therapy Using Interleukin-21-Primed Cytotoxic T-Cell Lymphocytes Combined With Cytotoxic T-Cell Lymphocyte Antigen-4 Blockade Results in Long-Term Cell Persistence and Durable Tumor Regression” and “Combined IL-21-primed polyclonal CTL plus CTLA4 blockade controls refractory metastatic melanoma in a patient,” were published in the Journal of Clinical Oncology and the Journal of Experimental Medicine, respectively.
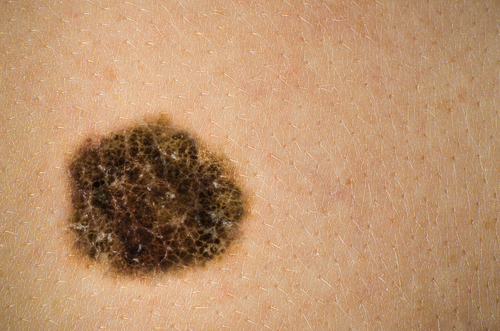
First author Dr. Aude Chapuis and colleagues harvested T-cells from 10 metastatic melanoma patients who did not respond to previous surgical or systemic therapy, as part of a Phase 1 clinical trial. They exposed these T-cells to melanoma-specific antigenic peptides (small molecules that activate immune T cells), such as MART1, to help them recognize tumor cells and destroy them.
In previous studies, when the T-cells were transferred back into the bodies of the patients, they did not perform as expected because the cells survived only about two weeks before they died. Now, in combination with MART1, scientists exposed the T-cells to the signaling molecule IL-21, which helps maintain cell renewal. They also used an immnune inhibitor (CTLA-4 inhibitor) to prevent tumor cells from silencing the T-cells.
When the cells were transferred back into the patients, two of the 10 subjects showed a complete remission of the melanoma that lasted for at least three years. Five other patients showed partial reduction in the number and volume of the tumors, or a halt in the progression of the disease.
When the scientists analyzed these patients more closely, they saw that the cytotoxic T-cells were still present in their blood even after 12 weeks following the transfer. The scientists speculated that the T-cells persisted longer because a specific sub-population was behaving like long-lived memory T-cells, maintaining the ability to replicate and ensure continued response to antigens over time.
The researchers believe the positive clinical response seen in patients might be due to “epitope spreading”: the transferred T-cells attack the melanoma cells and destroy them. This stimulates an inflammatory response and expands the variety of melanoma specific antigens to be presented to naive T-cells that in turn recognize other cancer antigens.
In fact, the team observed that the immune cells isolated from the two patients who were in complete remission responded to a variety of melanoma-specific antigens besides MART1, supporting their proposed model.
Researchers also wanted to understand why all patients did not respond to this therapeutic approach. They isolated T-cells from patients who did not respond to therapy and found they expressed a receptor called PD-1 on their surface, a protein that upon binding to its receptor, silences responses to T-cells. In fact some tumor cells produce PDL1 protein and evade the immune system in this way. This may partially explain why some patients do not respond to the therapy.
Scientists now think these “non-responder” patients may benefit from therapies that block PD-1 receptors in combination with CTLA-4 inhibition and T-cell “training.”
When T-cells are exposed to antigenic peptides they express different receptors on their surface. If the most common receptors expressed on the surface of T-cells from patients who respond well to treatment could be identified, these could be induced on the surface of the T-cells of non-responders using viral vectors, potentially ameliorating “outcomes in a larger subset of patients but also to be more feasible in terms of a Phase 2 trial,” Chapuis said in a press release.
Although very promising, these results are from a very small number of patients and cannot predict a general response from an entire population. Future larger-scale studies are necessary.


One comment