 A new treatment strategy combining radiation therapy and two immunotherapies that target the CTLA4 and PD-1 pathways was recently shown to induce an optimal response in patients with metastatic melanoma. The study entitled “Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer” was published in Nature by researchers at the University of Pennsylvania.
A new treatment strategy combining radiation therapy and two immunotherapies that target the CTLA4 and PD-1 pathways was recently shown to induce an optimal response in patients with metastatic melanoma. The study entitled “Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer” was published in Nature by researchers at the University of Pennsylvania.
The team performed the “RadVax” phase I clinical study where they evaluated the effect of combining ipilimumab and radiation in 22 metastatic melanoma patients that were previously treated or untreated. Ipilimumab is a monoclonal antibody that targets CTLA-4, a protein receptor that down-regulates the immune responses. Patients received stereotactic body radiation therapy (SBRT) to a single tumor followed by 3 to 5 days with ipilimumab every 3 weeks for 4 cycles.
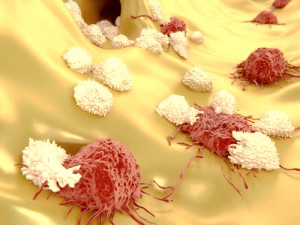
The research team found that this therapy was safe and decreased tumors in 18% of the patients. In parallel, the results in mice were similar to the clinical trial data with 17% of mice responding to the combined therapy, radiation therapy and an anti-CTLA4 antibody. Animal studies elucidated the mechanisms of resistance involving the PD-L1 pathway were due to increased levels of PD-L1 on melanoma cells and associated with T-cell exhaustion, a state were T cells are dysfunctional. In the lab, the authors inhibited PD-L1 restoring both T cell function and tumor response to radiation therapy and anti-CTLA4, with an increase survival of 60%. This finding suggests that an antibody targeting PD-L1 or its partner PD-1, like pembrolizumab or nivolumab, could be a perfect third treatment to ameliorate tumor response to radiation along with improved immunity.
Melanoma patients who exhibited high PD-L1 levels did not respond to radiation combined with anti-CTLA4, had sustained T-cell exhaustion and a rapid tumor progression. On the other hand, patients with low PD-L1 tumors showed a 50% survival.
The authors concluded that PD-L1 on tumor cells may be a central resistance mechanism to radiation therapy and ipilimumab (anti-CTLA4-based treatment). Therefore, optimal response and immunity in melanoma and other types of cancer will require radiation, anti-CTLA4 and anti-PD-L1/PD-1 inhibitors.
It has been suggested that tumor cells after radiation release antigens that “educate” the immune system to fight other tumors in the body. The therapy has been designated “RadVax” because of its vaccine-like properties. “This approach is changing the way we view radiation—from strictly a local form of therapy to one that may augment a systemic response when given with immunotherapy,” said study author Dr.Amit Maity.
Dr. Andy J. Minn added that understanding resistance is very important, but combining therapies can improve the treatment outcome. However, due to the possibility of advert effects, therapies should be tailored to the individual patient.
“These results are extremely encouraging and will allow us to propel the work further, into bigger clinical studies investigating the triple threat,” said Dr. Vonderheide, responsible for leading the clinical trial in other types of cancers, such as pancreatic, lung and breast.


