A new research study has found that malignant melanoma patients responded better to immunotherapy treatment when they had more diverse gut flora – microbes and bacteria that live in our guts.
The study was led by scientists at the University of Texas MD Anderson Cancer Center and presented at the National Cancer Research Institute’s (NCRI) Cancer Conference in Liverpool earlier this month, under the title “Enhancing responses to melanoma therapy with novel combinations of targeted therapy and immune checkpoint blockade.”
Immunotherapy is a promising avenue of cancer treatment because it harnesses the body’s immune system to target cancer cells. However, not everyone responds well to immunotherapy and researchers are trying to find out why.
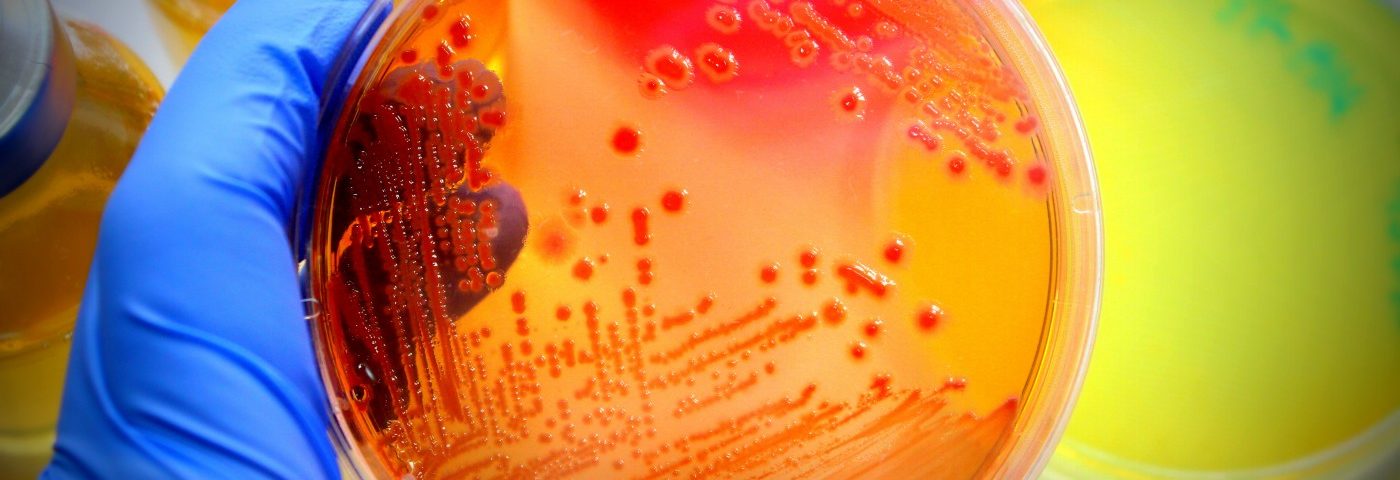
The research team studied more than 200 mouth and 100 gut microbiome samples from people with advanced melanoma. They discovered that those who recorded better responses to immunotherapy had more heterogeneous, or diverse, gut floras.
While no differences were found in the type of mouth bacteria between patients, the team found meaningful variances in the gut bacteria of people whose cancer responded better to treatment, as opposed to those whose cancer did not respond to immunotherapy.
“Our research shows a really interesting link that may mean the immune system is aided by gut bacteria when responding to these drugs. Not all patients respond to immunotherapy drugs and it’s hard to know who will benefit from the treatment prior to it being given,” Jennifer Wargo, MD, lead researcher at the University of Texas and co-author of this study, said in a press release. “The gut microbiome can be changed through a number of different strategies, so there is real potential here to modify the gut microbiome to boost an immunotherapy response,” she said.
Early studies in mice showed that changing the type of bacteria in the gut could improve the response to immunotherapy. This was the one of the first studies to look at the connection in human patients.
This study suggested that adapting people’s gut bacteria (with antibiotics, probiotics, or even fecal transplant) before immunotherapy could enhance the effectiveness of immunotherapy drugs. The authors of the study also pointed to the need of testing this hypothesis with new clinical trials.
“There is growing evidence that gut bacteria play a vital role in warding off disease, absorbing nutrients from the food we eat, and maintaining normal function of our immune systems,” said Pippa Corrie, PhD, chair of the NCRI’s Skin Cancer Clinical Studies Group. “Gut microbes have been shown to influence the role of conventional chemotherapy, so it’s probably not surprising that they impact on response to new immunotherapies being used in the clinic. Manipulating the gut flora may be a new strategy to enhance activity of immunotherapy drugs, as well as to manage problematic toxicity in the future,” Corrie said.