Keytruda (pembrolizumab), an imunotherapy used to treat advanced cancers, may have therapeutic effects in brain metastases of patients with melanoma and non-small cell lung cancer (NSCLC), as suggested by early results from an ongoing clinical trial.
Patients with untreated brain metastases are excluded from most clinical trials, and the effect on the central nervous system of most cancer drugs has not been well studied despite the fact that about 50,000 people with metastatic melanoma or NSCLC develop brain metastases annually in the U.S.
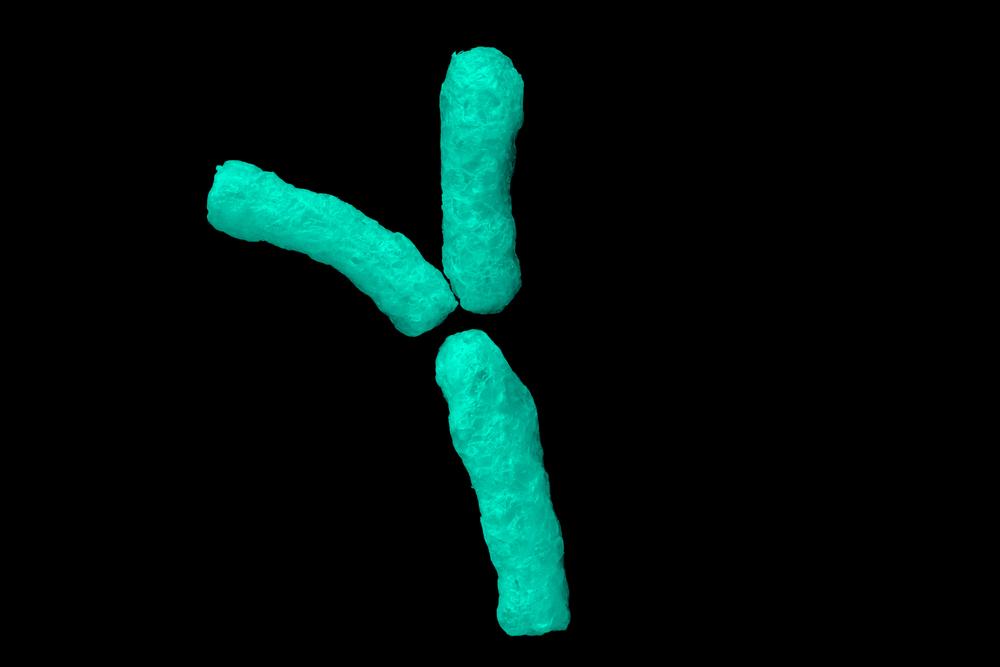
Keytruda works by inhibiting the programmed cell death ligand 1 (PD-L1), which normally binds and blocks to the programmed-cell death 1 receptor (PD-1) found on lymphocytes. Cancer cells that express PD-L1 can escape an effective immune response, and Keytruda allows the immune system to recognize and attack tumor cells.
During the randomized Phase 2 clinical trial “Pembrolizumab Plus Bevacizumab for Treatment of Brain Metastases in Metastatic Melanoma or NSCLC,” researchers administered 10 mg/kg of Keytruda intravenously every two weeks to 36 melanoma or NSCLC patients with untreated brain metastases.
All patients had brain metastases between 5 and 20 mm and exhibited neurological symptoms. PD-L1 expression was required for patients with NSCLC but not for patients with melanoma.
The results showed that 22 percent of melanoma patients and 33 percent of NSCLC patients had a brain metastasis response following treatment. There were some neurological effects associated with the treatment, and six melanoma patients and nine NSCLC patients died as a result of disease progression. The cause of death of one patient was unknown.
“Our findings clearly show that systemic PD-1 inhibition can be effective in treating nonirradiated or progressing brain metastases,” wrote Dr. Sarah B. Goldberg, assistant professor in the department of medical oncology in the Smilow Cancer Hospital at Yale School of Medicine, and her colleagues, according to a press release.
Data regarding overall survival, progression free survival and biomarkers are expected as the trial progresses.
According to the authors, the proportion of patients with melanoma who responded to treatment is relatively low in this study compared to other studies with Keytruda. This “might reflect complexities of clinical trials in this patient population” and “might underrepresent clinical benefit” of Keytruda, the authors wrote.
“Because new targeted treatments have prolonged survival in patients, and because whole-brain radiotherapy can impair memory, research into novel treatment for patients with brain metastases are warranted,” Dr. Rafael Rosell, director of the Cancer Biology and Precision Medicine Program at Catalan Institute of Oncology of Hospital Germans Trias i Pujol in Barcelona, Spain, and Dr. Niki Karachaliou, medical oncologist and a member of the Translational Research Group in Pangaea Biotech SA in Barcelona, Spain, wrote in an invited commentary.
“Treatment with anti–PD-1 antibodies is a promising new therapeutic approach that should be used in combination with targeted treatments to inhibit crucial oncogenic signaling pathways to prevent the absence of T-cell infiltrates in tumor sites,” they added.