 Over the last four years, a promising new class of cancer therapeutics has emerged in which an innovative method, coined immune checkpoint therapy, is exploited to seek and destroy tumors of advanced melanoma patients. While previous alternative therapies have focused on targeting the tumor itself, the goal of immune checkpoint therapy is to completely unleash the immune system, specifically the T cell response, to result in more efficient recognition and destruction of tumors. Due to its efficacy at the patient bedside, Drs. Sharma and Allison of M.D. Anderson Cancer Center suggest that immune checkpoint therapy has now become a viable alternative to classical melanoma treatments such as surgery, radiation, chemotherapy, and targeted therapies.
Over the last four years, a promising new class of cancer therapeutics has emerged in which an innovative method, coined immune checkpoint therapy, is exploited to seek and destroy tumors of advanced melanoma patients. While previous alternative therapies have focused on targeting the tumor itself, the goal of immune checkpoint therapy is to completely unleash the immune system, specifically the T cell response, to result in more efficient recognition and destruction of tumors. Due to its efficacy at the patient bedside, Drs. Sharma and Allison of M.D. Anderson Cancer Center suggest that immune checkpoint therapy has now become a viable alternative to classical melanoma treatments such as surgery, radiation, chemotherapy, and targeted therapies.
Over the last decade, scientists’ understanding of the molecular basis of cancer biology has grown tremendously and has led to several new strategies of cancer therapy. Targeted therapy is one such strategy and is characterized by the use of a drug to target tumors specifically. For instance, tumor formation and progression that is driven by the continuous activation of the BRAF signaling pathway would be treated by administering a drug that inhibits BRAF. While targeted therapies such as this have led to encouraging clinical outcomes, often these treatment responses are of relatively short duration. An advantage of targeted therapy, however, is the ability to utilize biomarkers to determine the specific tumor-associated anomaly that requires proper regulation.
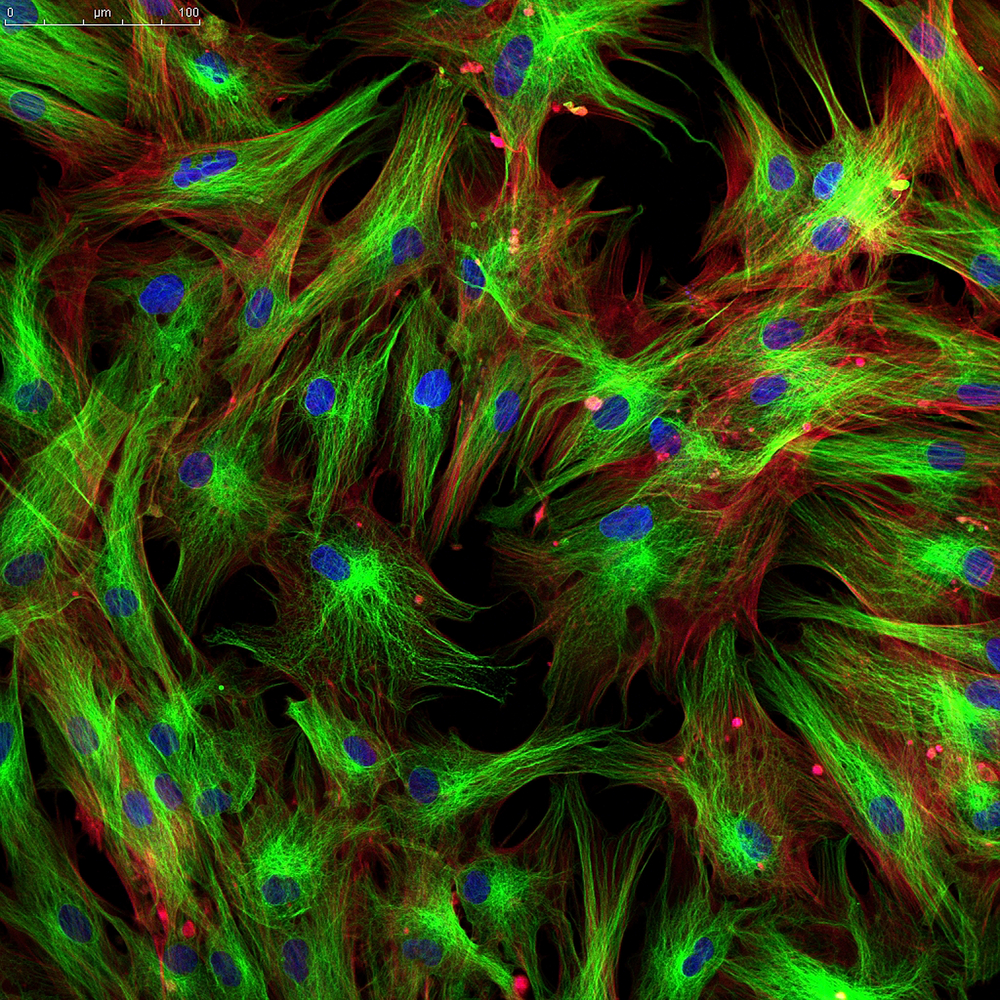
Immune checkpoint therapy, which is characterized by unleashing a T cell immune response, offers a promising alternative to targeted therapy in advanced melanoma patients. In addition to the many stimulatory and antagonistic mechanisms of T cell activation, T cell regulation is also comprised of post-activation checkpoints that can dampen the T cell immune response even after it has been activated. Immune checkpoint therapy aims to inhibit these aforementioned post-activation checkpoints, allowing for an exceedingly efficient T cell response and, ultimately, destruction of the tumor.
The expression of ctla-4 is one such checkpoint by which the efficiency of T cells is diminished post-activation. Therefore, scientists used antibodies against CTLA-4 to prevent this inhibitory checkpoint and increase T cell activation. This treatment was developed into a drug, ipilimumab, which was shown in clinical trials to generate enduring responses in advanced melanoma patients, by extending lifespan by four years, in about 20 percent of patients. Strikingly, ipilimumab increased the lifespan beyond ten years in a subset of patients. This was the first immune checkpoint therapy drug and was approved by the FDA in 2011 to treat advanced melanoma. Ipilimumab’s benefits may not stop at the treatment of advanced melanoma, as this drug was preliminarily shown to beneficially impact patients with renal cell carcinoma, prostate cancer, urothelial carcinoma, and ovarian cancer.
A second immune checkpoint gene, pd-1, has also been targeted in immune checkpoint therapy. Expression of pd-1 has been associated with a loss of T cell signaling, which, similar to ctla-4, corresponds to a dampened anti-tumor T cell response. However, it is important to note that these two genes function in different checkpoints of T cell regulation. As an alternative method of immune checkpoint therapy, researchers generated two separate drugs to target PD-1, pembroluzimab and nivolumab. Pembroluzimab led to advanced melanoma patients’ response rates of around 38%, with a 26% response rate in patients that had previously failed to respond to ipilimumab. Strikingly, nivolumab exhibited a 40% response rate and 73% survival rate of metastatic melanoma patients. While the FDA approved both of these drugs for the treatment of advanced melanoma in 2014, nivolumab was very recently approved for the treatment of advanced non-small cell lung cancer.
Due to the distinct mechanisms of action of both ipilimumab and nivolumab, combination therapy was tested to determine if increased efficacy could be achieved. Indeed, this was the case, as combinatorial therapy increased advanced melanoma tumor regression rate to around 80% in about half of the patients observed. This dramatic increase in tumor regression response rate highlights the impact and power of combinatorial therapy that can be utilized in immune checkpoint therapy.
However, improvements are still needed in the field of immune checkpoint therapy. First, immune checkpoints beyond that of CTLA-4 and PD-1 must be targeted. This would serve to further enhance the power of immune checkpoint combinatorial therapy. Second, while targeted therapies can benefit from biomarker identification as a method of selecting the most suitable therapy on a personalized patient level, immune checkpoint therapy falls short. Due to the overwhelming complexity and constant evolution of the immune response, the likelihood of identifying a single biomarker to identify the most suitable personalized therapy is low. Rather, researchers must identify a panel of biomarkers and define a standard by which to guide the combinatorial immune checkpoint therapy for each patient. In addition to this complexity, researchers must also be able to track changes in the tumor biomarker panel of a patient to assess if alterations in combinatorial therapies are necessary along the course of treatment.
Overall, while further research is needed to elucidate the full potential of immune checkpoint therapy, their ability to be applied in combination to dramatically increase tumor regression suggests that these treatments could one day be used to reliably control melanoma tumor progression. Furthermore, immune checkpoint therapy opens the door for other innovative methods of unleashing the full potential of the immune response in an effort to combat several other forms of cancer.