Inflammation is a process by which the immune system responds to a disease or injury. Chronic inflammation, however, has been linked to several types of cancers, such as basal cell carcinoma, lung, liver, colon cancer and others. Although this association is acknowledged, research has not been able to explain the cellular mechanisms that are involved in this process.
Inflammation is a process by which the immune system responds to a disease or injury. Chronic inflammation, however, has been linked to several types of cancers, such as basal cell carcinoma, lung, liver, colon cancer and others. Although this association is acknowledged, research has not been able to explain the cellular mechanisms that are involved in this process.
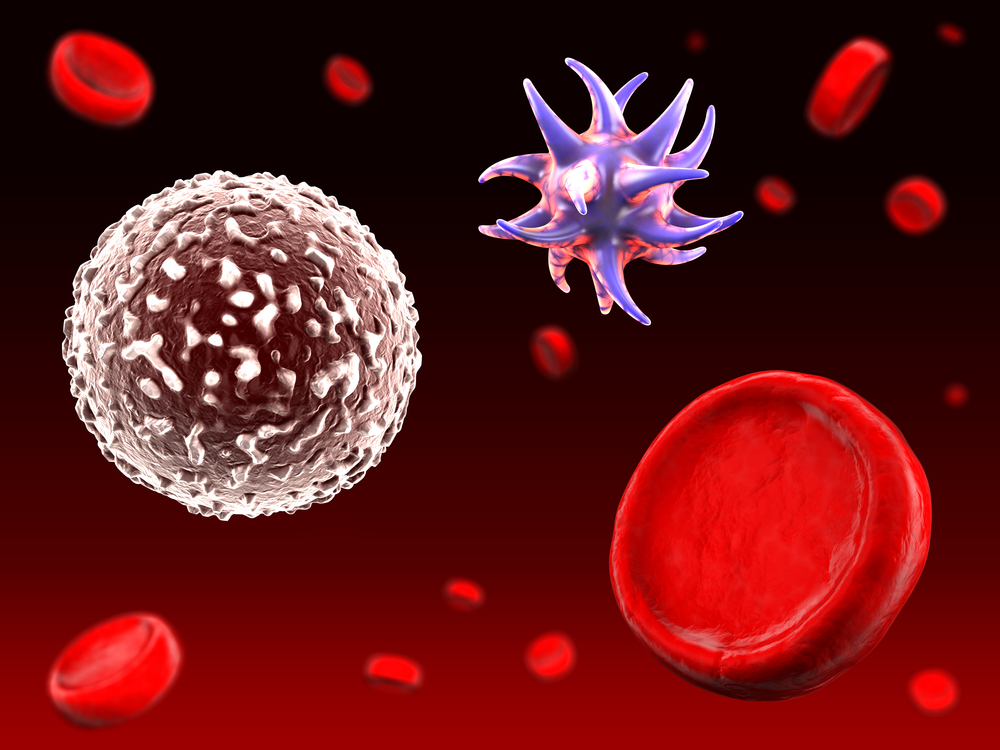
A new study entitled “Immature myeloid cells directly contribute to skin tumor development by recruiting IL-17–producing CD4+ T cells” was published in the Journal of Experimental Medicine by Dr. Myrna L. Ortiz, Dr. Vinit Kumar and Dr. Anna Martner, first co-authors, and led by Dr. Dmitry Gabrilovich from The Wistar Institute in Philadelphia, PA. In this study, researchers have shown that inflammatory conditions that favor the development of skin and colon tumors are linked to the accumulation of myeloid-derived suppressor cells in cancer tissues or to the accumulation of immature myeloid cells (IMCs) in individuals without tumors.
Dr. Dmitry Gabrilovich explained in a news release, that although it has been known for some time that genetic changes can lead to cancer, its also known that environmental factors are very important towards cancer development. “Inflammatory conditions are closely linked to cancer, yet it’s a very complex process, making it difficult to determine how certain components contribute to the development of cancer.” added Dr. Gabrilovich.
The research team used transgenic mice which provided the optimal conditions for local accumulation of immature granulocytic cells in the skin without the presence of an infection or tissue injury, the typical stimuli to induce inflammation. Upon topical application of 12-O-tetradecanoylphorbol-13-acetate (TPA), a common experimental carcinogen, in these mice there was a dramatic increase in the formation of papillomas, i.e. benign tumors, during epidermal carcinogenesis, correlating with the first signs of skin cancer. More importantly, the team found that immature myeloid cells (IMCs) arrive at the skin and stimulate the migration of T cells, which in turn stimulated the abnormal expansion of keratinocytes, the most frequent cell type found in the skin epidermis. Upon activation, IMCs produce a specific factor called CCL4, a chemokine that “recruits” T cells, mainly CD4+ T cells, to the skin. These CD4+ T cells produce interleukin-17 (IL-17), a proinflammatory cytokine, already shown to be associated with chronic inflammation and inflammatory tumors. The authors observed that removal of CD4+ T cells or inhibition of CCL4 or IL-17 stopped tumor formation as a consequence of IMCs.
Notably, the study identified a cascade of events that led to the development of skin cancer and also to the identification of novel potential therapeutic targets that could arrest the formation and development of skin cancer. Moreover, these results could be applied to other types of cancers caused by chronic inflammation. “If we are able to target these granulocytic cells directly, we may be able to prevent the inflammatory effects of IL-17, which would provide a great benefit to individuals with a high risk of developing these types of cancer,” concluded Dr. Vinit Kumar.