 An international research team led by Dr. Trever Bivona of the University of California San Francisco (UCSF) identified a protein responsible for melanoma drug resistance. The study, published online in Nature Genetics, indicates a strategy to enhance the response to drug treatment and patient survival.
An international research team led by Dr. Trever Bivona of the University of California San Francisco (UCSF) identified a protein responsible for melanoma drug resistance. The study, published online in Nature Genetics, indicates a strategy to enhance the response to drug treatment and patient survival.
Certain therapeutic approaches target genetic mutations in melanomas, such as in BRAF and RAS genes. The drugs shutdown a signalling pathway (MAPK-pathway) activated in mutated tumor cells. Initially, patients with BRAF– and RAS-mutant tumors respond to the drugs, but eventually they develop resistance to the therapy, which can arise from compensatory survival mechanisms in cancer cells that are not targeted by current drugs. In these situations, oncologists switch to alternative drug treatments.
In this study, the authors were capable of pinpointing one of the escape routes used by tumor cells. “Instead of trying to figure out why patients have developed resistance after it has emerged, we need to decipher what survival tactic tumor cells will be most dependent on when they are challenged with targeted therapy,” study’s senior, Trever Bivona, said in a news release.
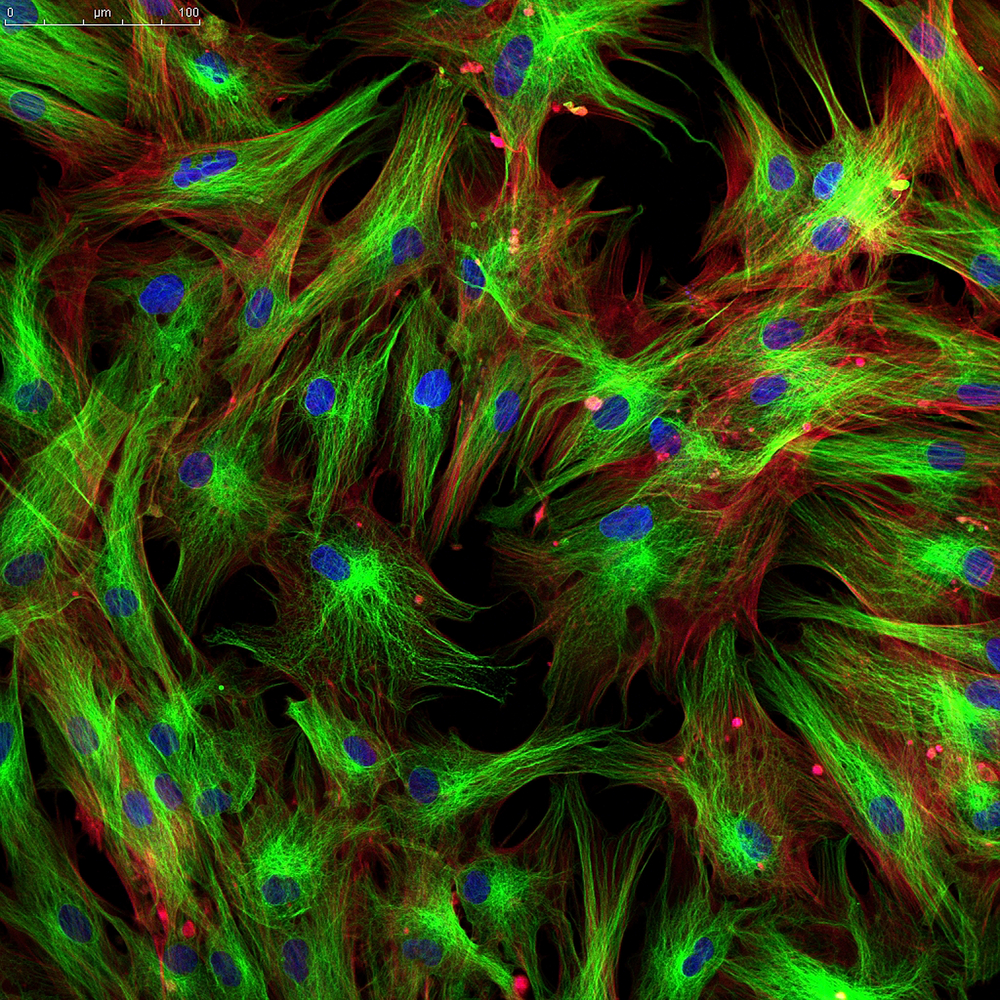
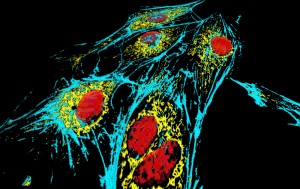
Researchers identified proteins whose absence in cancer cells bearing the BRAF or RAS mutations increased the response to Zelboraf and Mekinist, two currently used drugs in melanoma treatment. By reducing individual protein expression while treating the cells with the drugs, they identified those that, upon downregulation, allowed the drugs to become more effective.
The results showed a protein named YAP was responsible for drug resistance. This protein drives the growth of organs during development and regulates their size in adulthood. The result was unexpected: “YAP was the number-one hit in our screening process, but it wasn’t much of a leap to think it might be promoting resistance to targeted therapy, because it had been shown to promote organ growth and cell proliferation in other organisms and systems,” said Dr. Bivona.
Importantly, in animal models injected with melanoma cells, treatment was also more efficient upon absence of YAP.
Scientists found that increased YAP in BRAF– and RAS-mutant melanomas was a biomarker of worse initial response to drug treatment. Moreover, YAP levels rose in tumors when patients developed resistance to the therapy, demonstrating the clinical relevance of YAP-mediated melanoma drug resistance.
“This is the first paper to establish that YAP is a bona fide mechanism of resistance to RAF and MEK inhibition,” Bivona said, “and it’s exciting to contemplate and plan what we may be able to do with this knowledge to help cancer patients by improving their precision treatment,” added Dr. Bivona.