 Recent research has unveiled the mechanisms responsible for targeted therapy resistance in melanoma patients.
Recent research has unveiled the mechanisms responsible for targeted therapy resistance in melanoma patients.
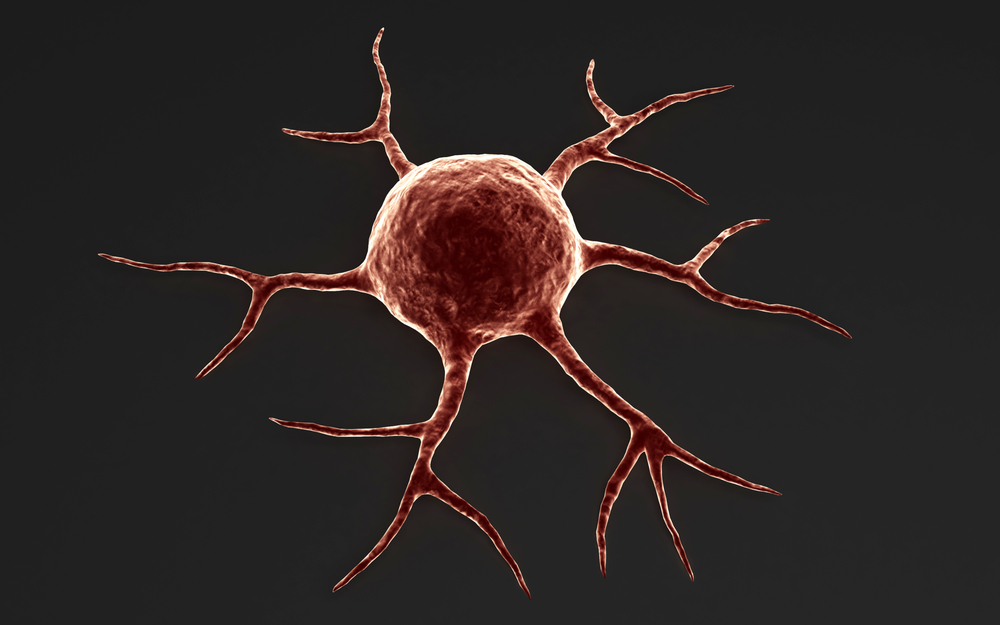
This type of therapy has a lower toxicity rate and can improve results for different types of cancers, bypassing several side effects associated with currently used chemotherapies. Nonetheless, patients usually acquire some degree of resistance to targeted therapies, allowing tumor cells to progress and become more aggressive, eventually acquiring a metastatic phenotype.
Proteins commonly found mutated in human cancers that facilitate tumor migration and survival, such as B-Raf and MEK, are the targets of several drugs, and have already proven efficient in clinical studies. In fact, combination therapy with B-Raf and MEK inhibitors is the standard of care in patients who are diagnosed with B-Raf positive melanoma. Nonetheless, throughout time these therapies become less efficient as patients acquire resistance to these inhibitors.
In this recent study, published in Cancer Discovery, researchers from Moffitt Cancer Center found that patients who are being treated with B-Raf inhibitor drugs can actually develop a higher number of metastases when compared to those on normal chemotherapy. This is due to the fact that melanoma cells resistant to B-Raf inhibitors have a more aggressive and invasive phenotype, allowing them to travel and colonize distant parts of the body.
Importantly, researchers found that this resistance was due to enhanced activity of EphA2, a cell surface protein present in tumor cells.
If resistant cells were withdrawn from B-Raf or MEK inhibitor drugs, their aggressiveness was reverted. “This suggests that alternate dose scheduling where B-Raf and MEK inhibitors are given to patients intermittently may reduce the aggressiveness of the disease… meaning patients could stay on therapy for more time,” Keiran S. Smalley, Ph.D., scientific director of the Donald A. Adam Comprehensive Melanoma Research Center of Excellence at Moffitt, said in a news release.
Furthermore, when the team specifically targeted the EphA2 protein, it led to a significant decrease in the metastatic behavior of melanoma cells, suggesting that a drug targeting this protein will have the capacity to prevent therapy resistance and the development of new malignancies in patients undergoing B-Raf and B-Raf /MEK inhibitor therapy.