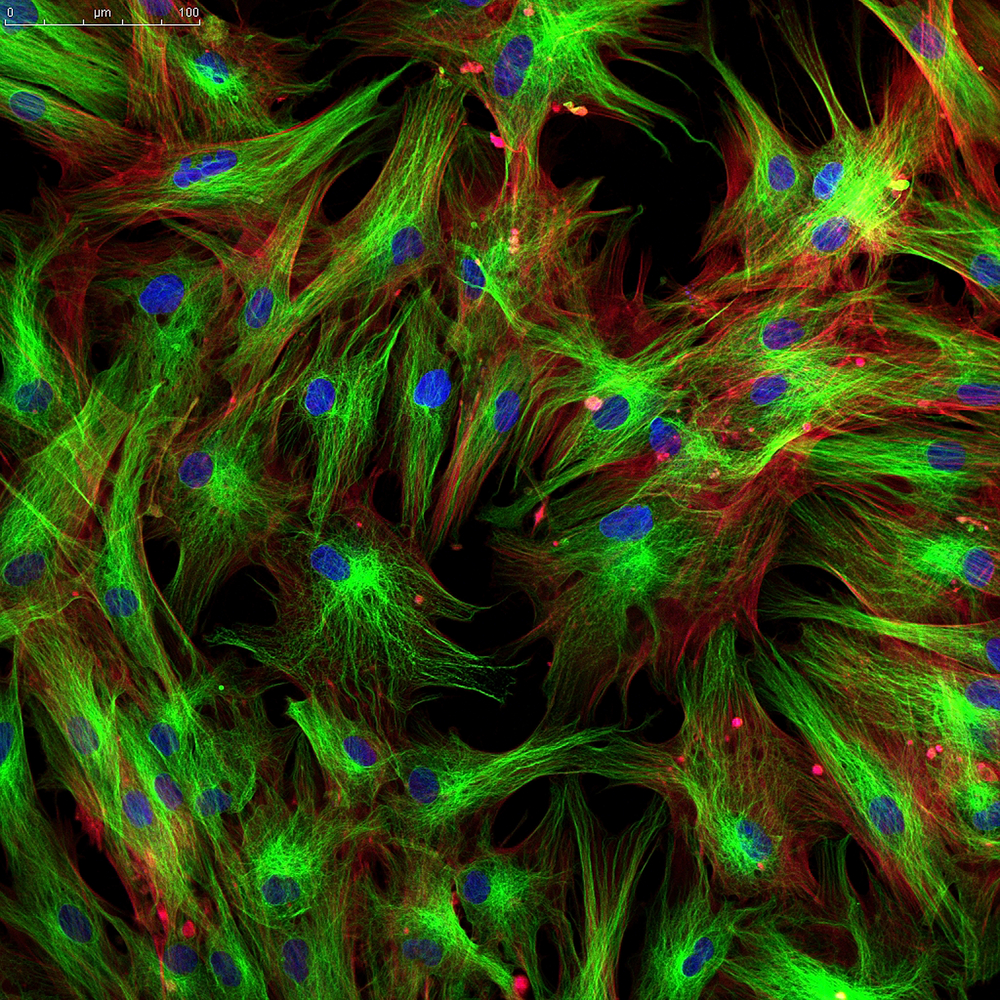
 A new study established a way to convert fibroblasts into functional melanocytes, the body’s pigment-producing cells. The study entitled “Direct conversion of mouse and human fibroblasts to functional melanocytes by defined factors”was published in Nature Communications by Dr. Ruifeng Yang Perelman School of Medicine, University of Pennsylvania and colleagues.
A new study established a way to convert fibroblasts into functional melanocytes, the body’s pigment-producing cells. The study entitled “Direct conversion of mouse and human fibroblasts to functional melanocytes by defined factors”was published in Nature Communications by Dr. Ruifeng Yang Perelman School of Medicine, University of Pennsylvania and colleagues.
The technique established in this work will likely have important outcomes for the development of novel cell-based therapies for skin conditions like vitiligo and for screening strategies for melanoma.
“Through direct reprogramming, we do not have to go through the pluripotent stem cell stage, but directly convert fibroblasts to melanocytes. So these cells do not have tumorigenicity”, senior author Dr. Xiaowei “George” Xu said in a press release.
As an organism develops from the embryonic state to a fully developed adult state, cells divide and differentiate. Researchers have developed stem cell therapies which allows them to obtain cells with the ability to acquire a specific function and be used for novel treatments.
It has been very difficult to establish the key transcription factors to obtain a specific type of cell. Moreover, the process to convert a cell into an induced pluripotent stem cell (iPSC), with the ability to differentiate into a specific cell type can result in unexpected tumor growths.
The research team identified 10 specific cell transcription factors important for melanocyte development. They then preformed a transcription factor screening assay and identified 3 transcription factors that are important for melanocytes: SOX10, MITF, and PAX3, a combination dubbed SMP3.
“We did a huge amount of work,” said Dr. Xu “We eliminated all the combinations of the other transcription factors and found that these three are essential,” he added.
The research team used a combination of SMP3 and mouse embryonic fibroblasts, observing that embryonic fibroblasts started to display melanocytic markers. Furthermore, the team used a SMP3 from human origin together with human fetal dermal cells, and obtained melanocytes (human-induced melanocytes, or hiMels). These hiMels behaved functionally as normal melanocytes, produced melanin pigment, both in vitro and in animal models.
Dr. Xu said that this method of developing melanocytes from melanoma patients’ fibroblasts could be a novel way to investigate into this malignancy. “We can screen not only to find why these patients easily develop melanoma, but possibly use their cells to screen for small compounds that can prevent melanoma from happening”, Dr. Xu explained.
The researchers highlighted there are a lot of fibroblasts present in the body that could undergo cell reprogramming, contrary to tissue-specific adult stem cells, which are not so abundant, making this method highly adequate for other cell-based treatments.