 A new study addressing the effect of highly focused radiation in boosting the immune system to target and kill cancer cells upon combination with a novel type of immune-enhancing drug, was presented last week at the 2014 annual meeting of the American Society of Radiation Oncology (ASTRO) in San Francisco.
A new study addressing the effect of highly focused radiation in boosting the immune system to target and kill cancer cells upon combination with a novel type of immune-enhancing drug, was presented last week at the 2014 annual meeting of the American Society of Radiation Oncology (ASTRO) in San Francisco.
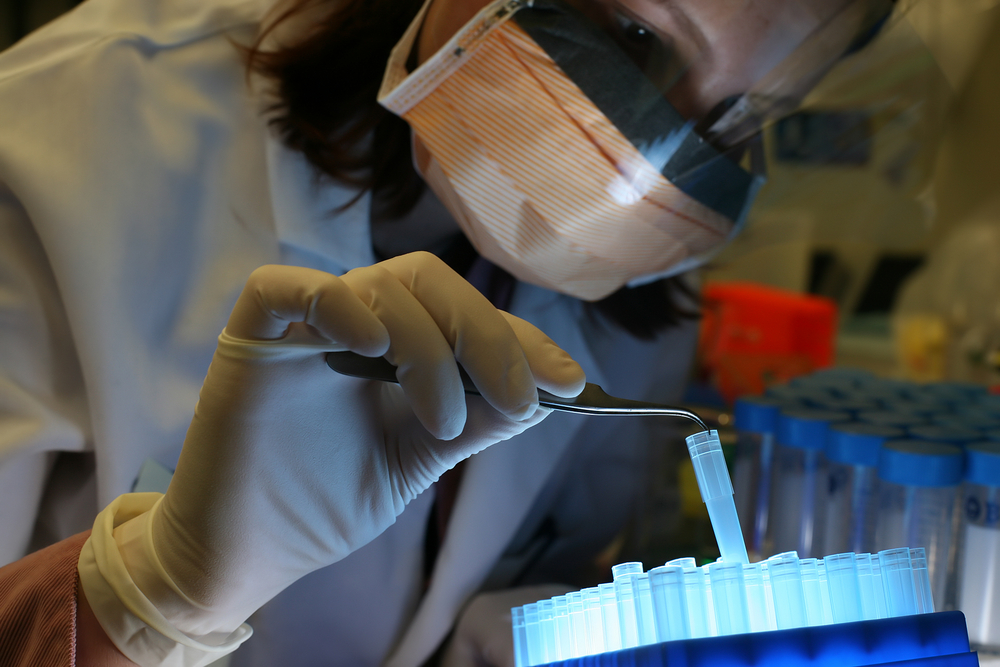
Dr. Andrew Sharabi, M.D., Ph.D., a resident in the Department of Radiation Oncology and Molecular Radiation Science at Johns Hopkins and colleagues, used animal models of melanoma and breast tumors, to study the synergetic effect of radiation with a novel class of anticancer agent, pembrolizumab, that enhances the ability of the immune system to recognize cancer.
Pembrolizumab, a “checkpoint inhibitor” with the trade name Keytruda (Merck), is a monoclonal antibody that targets the programmed cell death 1 (PD-1) receptor, an inhibitory receptor that behaves as an immune checkpoint and prevents uncontrolled immune reactions, interfering with the capacity of the immune system to recognize and kill tumors. This drug is planned to be used in metastatic melanoma treatments, and was recently approved by the U.S. Food and Drug Administration (FDA).
“The immune system has powerful brakes, and removing those brakes with checkpoint inhibitors may be key to unleashing the full potential of the immune system against cancer,” Dr. Sharabi stated in a Science Daily article. “Adding radiation therapy to this mix may provide an additional boost by increasing tumor cell death and releasing targets for the immune system. We found that focused radiation therapy, once thought to suppress the immune system, actually increases specific, antitumor responses from the immune system,” added Dr. Sharabi
“The increased immune cell division in lymph nodes suggests that radiating the tumor seems to activate immune cells in the surrounding lymph nodes, not just the tumor,” Dr. Charles Drake, M.D., Ph.D., associate professor of oncology and medical oncologist at the Johns Hopkins University School of Medicine and the Kimmel Cancer Center explained in the press release.
Furthermore, the researchers observed an increase in memory T-cells, a specific type of T-cell that can retain tumoral memory, in mice treated with the combined immunotherapy-radiation therapy. “This may help stem recurrence of cancer.” emphasized Dr. Sharabi.
Importantly, to assess memory building by the immune system, the team transferred immune cells isolated from mice treated with the combination therapy into normal mice, and proceeded to implant new tumors under the skin of these mice. “The transferred immune cells inhibited growth of the tumors, suggesting that the immune cells can travel throughout the body and attack sites outside of the radiation field,” stated Dr. Sharabi.
Moreover, to understand the mechanism by which the radiation boosted the immune system, Dr. Sharabi explained that, “Radiation causes damage to cancer cells, and the cells produce molecules called chemokines that can help to recruit an immune response.”
Currently, the research team is performing more studies to assess the optimal radiation dose and timing needed to generate the best immune response.