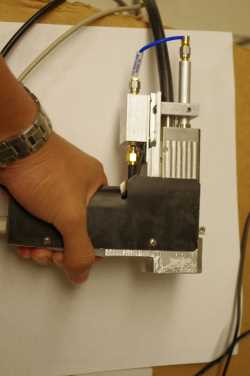
Researchers from Washington University in St. Louis have constructed a hand-held photoacoustic microscopy device that uses lasers and sound waves to measure how deep a melanoma tumor extends into the skin. This can provide crucial information, revolutionizing the current approaches used by doctors to treat and diagnose melanoma.
Researchers from Washington University in St. Louis have constructed a hand-held photoacoustic microscopy device that uses lasers and sound waves to measure how deep a melanoma tumor extends into the skin. This can provide crucial information, revolutionizing the current approaches used by doctors to treat and diagnose melanoma.
In the study entitled “Handheld photoacoustic microscopy to detect melanoma depth in vivo”and published in the Optics Letters journal, the team tested their device in vitro on artificial tumors and in vivo using mice models of melanoma, showing the instrument could successfully measure melanomas with 4.1 and 3.7 mm thicknesses in living tissue.
The mechanism behind this newly developed technique relies mostly on a photoacoustic effect whereby light can be converted into vibration. A laser beam is projected directly towards the tumor, and melanin (skin pigment) absorbs this light, whose energy is then converted into high-frequency acoustic waves, which do not disperse when travelling through skin.
Because melanoma cells produce higher levels of melanin than the surrounding healthy tissue, these acoustic waves can produce a kind of map delimiting the entire tumor area. Furthermore, the device is endowed with software that can transform this information into a 3D image on a computer screen.
The problem with current techniques is that they can’t directly measure a tumor with accuracy, since light is scattered throughout the skin and cannot penetrate deep into the tissues. “None are really sufficient to provide the two to four millimeter penetration that’s at least required for melanoma diagnosis, prognosis or surgical planning,” engineer Lihong Wang, coauthor of the paper said in an Optical Society press release.
Moreover, due to the small size of a skin biopsy, it may not be possible to measure tumor depth, many times leading patients to preform a second excision if the surgeon finds that the tumor is deeper than initially predicted.
The chances of a melanoma tumor to become metastatic and deadly increase the thicker it becomes. To be able to measure the depth of the tumor in vivo provides a powerful tool to determine prognoses earlier, more accurately and to plan suitable treatments. Additionally, this instrument can measure a tumor’s entire volume, allowing for correlations on how tumor volume can relate to cancer outcomes.
In the near future, this device will be used solely for doctors to improve planning and surgery preparation, however, the researchers envision it can become available for commercialization after testing in clinical trials.