 A team of researchers from the Walter and Eliza Hall Institute, Melbourne have found that myeloid cell leukaemia sequence-1 (Mcl1) is crucial for the survival of natural killer (NK) cells in vivo, that in turn can clear melanoma cells that have spread to the lungs.
A team of researchers from the Walter and Eliza Hall Institute, Melbourne have found that myeloid cell leukaemia sequence-1 (Mcl1) is crucial for the survival of natural killer (NK) cells in vivo, that in turn can clear melanoma cells that have spread to the lungs.
Metastatic melanoma is a fatal disease with a rapid systemic dissemination and patients showing lung metastases usually have a 1-year survival of 57%.
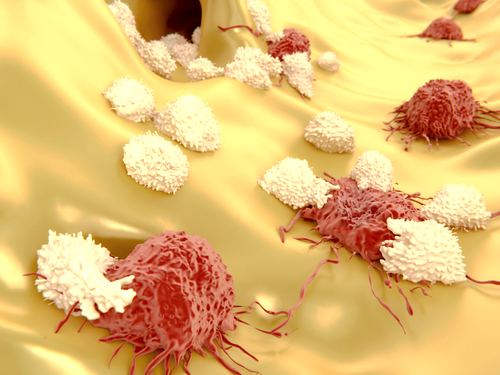
NK cells are a type of cytotoxic lymphocyte present at high frequencies in our blood and are responsible for rapid immune responses to virally infected cells and to tumor formation.
These cells usually reside in the lungs, intestines, mucous membranes and skin, where they can detect and destroy diseased cells.
The study entitled “Innate immunodeficiency following genetic ablation of Mcl1 in natural killer cells” and published in Nature Communications, showed that Mcl1 was highly expressed in NK cells and was regulated by IL-15, a cytokine that induces cell proliferation, via STAT5 phosphorylation.
The researchers developed a mouse model carrying a specific deletion of Mcl1 in NK cells, resulting in a total depletion of these cells from all the tissues, leading to multiorgan melanoma metastases in the genetically modified mice. Furthermore, NK lymphopenic mice were permissive to allogeneic transplantation as well as toxic shock upon polymicrobial sepsis challenge.
“We discovered MCL-1 is absolutely essential for keeping natural killer cells alive. Without natural killer cells, the body was unable to destroy melanoma metastases that had spread throughout the body, and the cancers overwhelmed the lungs. Knowing how important natural killer cells are for detecting and destroying cancer cells as they spread suggests they would be a good target for boosting immune defenses to treat cancer”, Dr Nicholas Huntington, senior author of the study, said in the institute’s press release.
The results from this research demonstrated that NK cells are responsible not only for donor stem cell rejection in bone marrow transplantations but also for production of inflammatory signals that could result in fatal sepsis.
Furthermore, experimental manipulation of the MCL-1 protein can possible lead to new and improved therapies targeting metastatic melanoma.